Where is liver pain felt? Knowing the answer helps you take the necessary action. It sits under your right rib cage and can cause different sensations when irritated or swollen. Sometimes, liver pain is obvious, but often it’s subtle and easy to mistake for indigestion, muscle strain, or gallbladder pain.
Let’s walk through where liver pain is felt, what it might mean, and what you can and should do if you feel. If you feel a sudden severe pain, yellowing of the skin or eyes, or confusion, please seek immediate medical care.
Where Is Liver Pain Felt in the Body?
The most common location for liver-related discomfort is the upper right portion of the abdomen, just under the rib cage, where the liver is. When it becomes inflamed, stretched, or enlarged it often produces a dull, heavy ache or a persistent pressure in that area.
That said, not every issue that causes right-upper-quadrant pain comes from the liver, and not all liver problems cause intense or obvious pain. Some liver conditions are “silent” for long periods or cause vague discomfort, while others produce definite, persistent tenderness. Use the location as a guide, but also note the quality of the sensation, timing, and any other symptoms you may have, like jaundice, fever, nausea, to get the whole picture.
What Does Liver Pain Feel Like?
Liver pain is most commonly described as a dull ache, a sense of fullness, or a deep pressure under the right ribs. It may feel constant or come and go with activity, meals, or changes in body position. It tends to be more diffuse, like a heavy tightness that doesn’t respond to antacids or rest. This difference helps distinguish it from other causes like acid reflux or muscular strain.
In some cases, the liver can also cause cramping, aching that increases after large or fatty meals, or a vague soreness that’s worse at the end of the day. Other clues that might accompany the sensation, like tiredness, mild nausea, or loss of appetite, point to a metabolic or inflammatory process rather than a simple belly cramp. Paying attention to these patterns helps both you and your doctor narrow down possible causes.
Where Is Liver Pain Felt Below the Rib Cage?
Because the liver sits directly beneath your right rib cage, tenderness or a sense of pressure below the right ribs is a classic placement for liver discomfort. You might notice it under the lowest ribs on the right side, or extending slightly toward the center of the abdomen depending on the liver’s size and which part is affected. Pressing gently under the right rib cage may reveal some sensitivity, but absence of tenderness doesn’t rule out liver problems, especially early on.
An enlarged liver (hepatomegaly) pushes against surrounding tissues and the rib cage, creating that feeling of fullness or discomfort. If swelling is present, you may also observe a subtle bump under the ribs or a broader area of tenderness.
Liver Pain vs Gallbladder Pain

Liver pain and gallbladder pain often overlap in location, both being present in the upper right abdomen, but they usually have different patterns and triggers. Gallbladder pain (or biliary colic) is often sharp, severe, and episodic, frequently beginning after a fatty meal and sometimes radiating to the right shoulder or back; it may come on suddenly and then fade over hours. Liver pain, by contrast, more commonly presents as a sustained, dull ache or pressure and is related to inflammation, swelling, or longer-term disease processes rather than an acute duct obstruction.
Associated symptoms help separate the two: gallbladder issues often produce intense pain with nausea and vomiting and may follow predictable episodes, whereas liver conditions are more likely to cause systemic signs such as fatigue, jaundice, dark urine, or abnormal blood tests. That said, there are exceptions and overlap as both organs share nearby anatomy and nerve pathways. Diagnostic tests (bloodwork and imaging) are often necessary. If you’re unsure which one it might be, keep track of timing, meal triggers, and any color changes in stool or urine and bring this information to your doctor.
Where Is Liver Pain Felt in the Shoulder Blade?
Yes, sometimes liver or gallbladder irritation is felt as pain in the right shoulder blade or the top of the shoulder. This is called referred pain and occurs because the diaphragm, which lies between the liver and the chest cavity, shares nerve pathways (notably via the phrenic nerve) that project to the shoulder area. When the diaphragm or the surface of the liver is irritated, the brain can interpret that signal as pain in the shoulder region even though the problem originates below the ribs. It’s one of those puzzling body tricks that can make diagnosis tricky unless you know to look for it!
If your shoulder-blade pain is accompanied by right upper abdominal discomfort, nausea, or any signs of systemic illness, that raises the likelihood it’s referred pain from the liver or gallbladder. Conversely, if the shoulder pain is clearly linked to movement, lifting, or a fall, it’s probably musculoskeletal. Noticing whether the shoulder pain spikes with breathing, coughing, or after eating can help you and your clinician figure out the source.
Where Is Liver Pain Felt After Eating?
For some people, liver-related discomfort becomes more noticeable after large or fatty meals. The liver and gallbladder are closely tied to digestion: a fatty meal prompts bile release and metabolic activity that can irritate the biliary system or reveal underlying liver stress. If you consistently feel upper-right fullness, bloating, or a dull ache after eating, especially fatty foods or alcohol, that pattern is an important clue that digestive triggers play a role in your symptoms.
Take note that while food-related timing is a strong signal for gallbladder disease, it can also reveal liver problems in people who have underlying inflammation or fatty change, the added digestive load simply makes symptoms more obvious. Keeping a simple food-and-symptom diary for a few days (what you ate, when pain started, how long it lasted) can be a surprisingly helpful diagnostic tool when you discuss the issue with your clinician.
Special Situations: Children and Pregnancy

Children and teenagers can experience liver-related problems but often present differently. Younger kids may describe general belly pain, feel unwell, lose appetite, or have jaundice that a parent notices before a child reports pain. Some pediatric liver issues are viral (like hepatitis A or B), metabolic, or occasionally related to systemic illnesses, and young children may not localize the discomfort to the right upper quadrant. If your child seems unusually tired, has persistent abdominal symptoms, or their eyes/skin look yellow, seek medical evaluation promptly.
During pregnancy, liver pain or any right-upper-quadrant discomfort should be taken seriously because pregnancy-specific liver disorders exist. Conditions such as intrahepatic cholestasis of pregnancy (ICP), acute fatty liver of pregnancy (AFLP), and HELLP syndrome are important to recognize: they can cause itching, upper abdominal pain, abnormal blood tests, and in some cases are urgent for maternal and fetal health. If you’re pregnant and notice persistent RUQ pain, intense itching (especially of the palms/soles), jaundice, or sudden swelling, contact your obstetrician or emergency care right away.
Liver Pain in Common Diseases
Different liver diseases tend to produce different patterns: fatty liver disease commonly produces a vague, dull discomfort in the upper right abdomen and often develops silently; viral hepatitis can cause pain, fatigue, dark urine, and jaundice depending on disease stage; liver cysts, abscesses, or tumors may cause focal pressure or sharp pain when they grow or become inflamed. Chronic conditions such as cirrhosis can cause persistent fullness or discomfort as the organ’s structure changes and the portal system is affected. Recognizing the pattern helps focus diagnostic tests.
The presence of systemic signs like fever, weight loss, jaundice, swollen abdomen from fluid (ascites), or altered mental status points toward more serious liver involvement and should prompt urgent assessment. Many liver conditions are diagnosed with targeted blood tests (liver enzymes, bilirubin), imaging (ultrasound, CT), and sometimes specialist referral; early detection often allows for much more effective treatment or lifestyle intervention.
Early Signs of Liver Pain
Early liver problems can be subtle: a low-level, persistent ache in the upper right abdomen, increasing fatigue, mild nausea, or general malaise are common early clues. Because the liver is resilient and can compensate for injury, symptoms may appear slowly and be easy to ignore, that’s why many liver diseases are described as “silent” until they’re advanced. Noticing a new, consistent discomfort in the RUQ that doesn’t respond to typical remedies is an early warning sign worth checking out.
Keep an eye out for accompanying early systemic signs such as reduced appetite, unexplained tiredness, pale stools, dark urine, or mild jaundice; these increase the likelihood that the liver is involved. Acting early like getting simple bloodwork and an ultrasound if recommended can identify problems when they’re easier to treat. If you have risk factors (obesity, diabetes, heavy alcohol use, or known viral hepatitis exposure), be especially vigilant.
Home Remedies for Temporary Relief

If your liver-related discomfort is mild and you’re waiting for an appointment, a few conservative measures can ease symptoms temporarily: avoid alcohol and heavy or fatty meals, stay well-hydrated, rest, and use gentle heat (a warm compress) to relax the area if it feels muscular. Over-the-counter pain relievers should be used cautiously, like acetaminophen (paracetamol), which can be harmful to the liver in high doses. Consult a clinician before taking anything regularly. Simple lifestyle adjustments often reduce irritation and can be very effective when the underlying issue is metabolic (like fatty liver).
Remember that these are temporary comfort measures, not cures. If the pain is severe, worsening, or accompanied by worrying signs (fever, jaundice, vomiting, fainting), stop home treatment and seek care right away. Home remedies are for comfort while you pursue a proper diagnosis and treatment plan. Be safe and conservative about medications!
At-Home Liver Health Checks You Can Try
You can perform a simple at-home liver test that may hint at liver involvement: look for yellowing of the skin or the whites of the eyes (jaundice), note dark urine or pale stools, check for persistent itching (especially on palms and soles), and keep track of fatigue and appetite changes. These signs aren’t definitive, but they’re important to mention to your provider and can help prioritize testing. For infants and young children, watch for poor feeding, excessive sleepiness, or high-pitched crying along with any yellowing, which are red flags and require immediate medical attention.
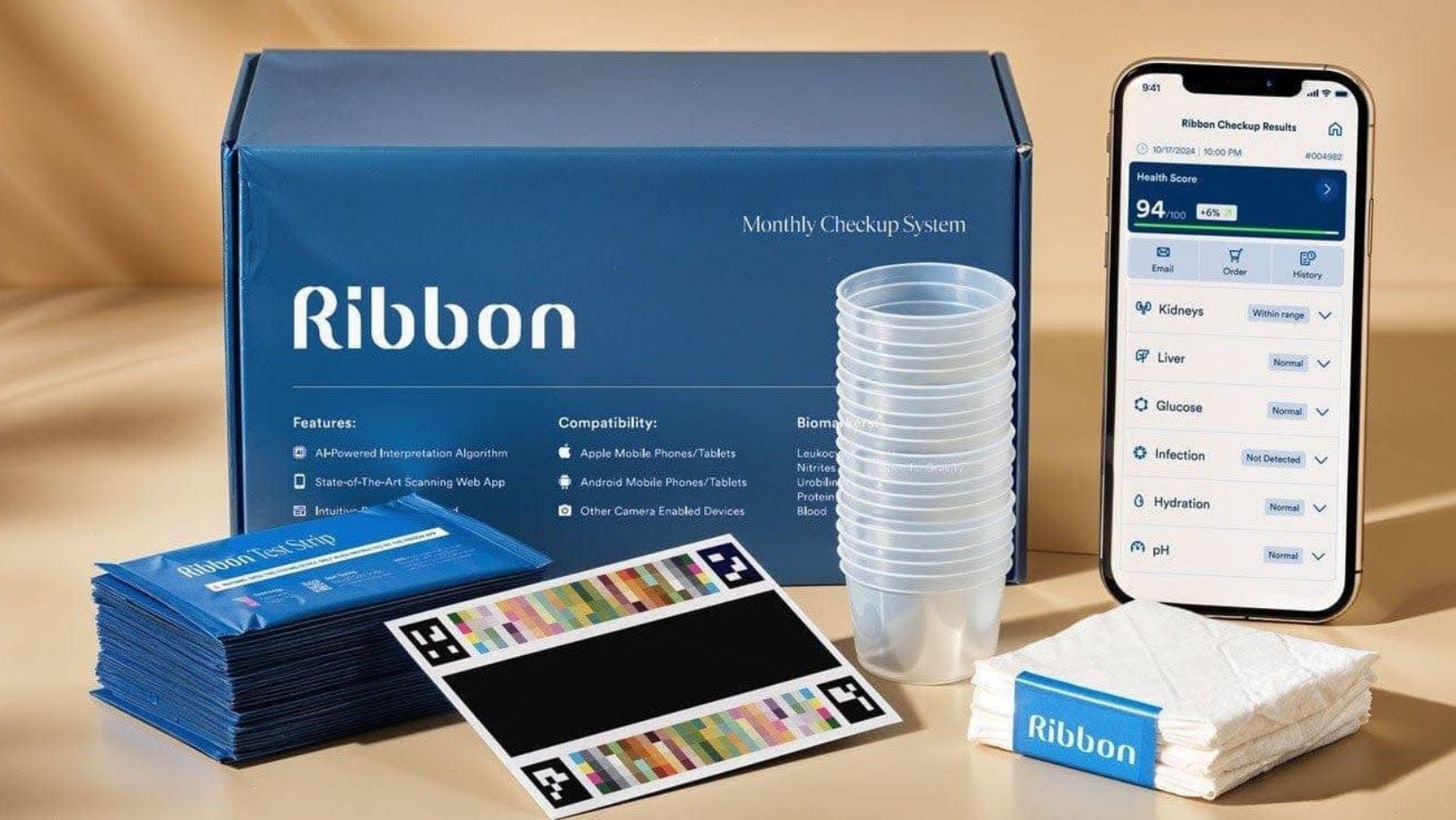
At-home test kits are increasingly available and can measure liver markers (like ALT, AST, bilirubin) from a finger-prick blood sample that you send to a lab; others provide basic urine tests. These kits can be useful as a screening tool or for monitoring, but they don’t replace formal laboratory testing, physical exam, and imaging. If a home test raises concerns, follow up quickly with a clinician for confirmatory testing and interpretation. Remember, home results are a starting point, not a diagnosis.
Lifestyle Tips to Support Liver Health
Whether you’re managing a diagnosed liver condition or trying to prevent one, lifestyle matters a lot. Aim for a balanced diet focused on whole foods, plenty of vegetables, lean proteins, and limited processed sugar and saturated fats; regular physical activity, weight management, and avoiding smoking or unnecessary medications will all support liver function. If you drink alcohol, follow safe consumption guidelines or consider abstaining if you have liver disease since alcohol is a common, modifiable contributor to liver injury.
Don’t neglect routine healthcare: vaccinations (for hepatitis A and B where appropriate), screening for metabolic risk factors (like diabetes and high cholesterol), and regular checkups can catch problems early. Small, consistent changes produce meaningful results for liver health over months and years. Celebrate incremental wins: reducing sugary drinks or adding regular walks matters!
When to See a Doctor
Seek immediate medical attention for severe or rapidly worsening pain, high fever, confusion, fainting, or any yellowing of the skin or eyes as these can indicate serious liver injury or complications. Also contact your clinician if you have persistent RUQ pain that lasts several days, unexplained weight loss, persistent nausea/vomiting, or new swelling of the abdomen or legs. In pregnancy, any RUQ pain or intense itching deserves urgent evaluation due to pregnancy-specific liver conditions.
For non-emergent but concerning symptoms, schedule a prompt appointment and bring a clear symptom timeline: onset, triggers, anything that helps or worsens the pain, medication or supplement use, alcohol history, and any recent travel or exposures. Clear communication speeds diagnosis and improves the chance you’ll get the right tests (bloodwork, ultrasound) quickly.
How Liver Pain Is Diagnosed

Clinicians use a combination of history, physical exam, blood tests, and imaging to diagnose liver problems. Initial bloodwork often includes liver enzymes (ALT, AST), bilirubin, alkaline phosphatase, and tests of clotting and proteins; these markers show whether the liver is inflamed, obstructed, or failing to perform certain functions. Ultrasound is a common first-line imaging test because it’s safe, painless, and effective for identifying enlargement, fatty change, gallstones, and many structural problems; more advanced imaging (CT, MRI) or biopsy may follow in complex cases.
Don’t be surprised if diagnosis takes a few steps — the liver is connected to metabolic, infectious, and structural processes, and narrowing down the cause sometimes requires sequential testing. If home testing or initial bloodwork flags abnormalities, your clinician may refer you to a hepatologist (liver specialist) for targeted evaluation and management. Prompt, stepwise testing helps avoid unnecessary procedures and gets you the right treatment faster.
Conclusion
To sum up: liver-related discomfort is most commonly felt in the upper right abdomen under the ribs, and it may radiate to the back or right shoulder blade through nerve referral. The quality is often a dull, persistent ache or a feeling of fullness rather than sharp, stabbing pain, though exceptions exist and overlap with gallbladder, stomach, kidney, and musculoskeletal causes is common. If you notice persistent symptoms, any yellowing of the skin or eyes, severe pain, or confusing systemic signs, seek prompt medical attention!
You don’t have to manage uncertainty alone: start with observation (a symptom diary), consider a safe at-home screening kit if that helps you act sooner, and follow up with a clinician for confirmatory tests. Early recognition and sensible lifestyle steps can prevent progression in many liver conditions.
